Testing positive for COVID-19 can be a daunting experience and it is essential to understand what the results mean. When a person is tested for COVID-19, the test aims to detect the presence of the SARS-CoV-2 virus, which is the virus that causes COVID-19. A positive test result indicates that the virus’s genetic material was found in the person’s sample, implying that the person is currently infected with the virus and could potentially transmit it to others. It’s crucial to note that a positive result does not necessarily denote severe sickness; the infection’s intensity can range from being asymptomatic (no symptoms) to severe, depending on a variety of factors such as age, underlying health conditions, and immune response. Following a positive result, it is advised to self-isolate and seek medical guidance promptly. Contact tracing should be initiated to alert those who have been in close contact with the infected individual, enabling them to take necessary precautions. Understanding the implications of a positive COVID-19 test result is pivotal in managing the disease and mitigating its spread.
What does a positive result on COVID-19 mean?
A positive result on a COVID-19 test indicates that the individual has been infected with the SARS-CoV-2 virus, the causative agent for the ongoing global pandemic. This outcome does not necessarily suggest that the person is currently ill or will become ill, but rather that they carry the virus and can potentially transmit it to others. A positive result is derived from a diagnostic test, commonly a PCR (Polymerase Chain Reaction) test, that identifies the genetic material of the virus in samples collected from the person’s respiratory system.
The severity of the symptoms differs significantly among individuals, ranging from asymptomatic cases, where there are no observable signs of the disease, to severe cases, which may require hospitalization. Individuals who test positive are advised to isolate themselves to prevent the spread of the virus to others. It’s essential to note that even asymptomatic individuals can spread the virus, emphasizing the importance of isolation following a positive result.
The interpretation of a positive result should also take into account the individual’s recent contacts, symptoms, and the prevalence of the virus in the community. For example, in a population where virus transmission is rampant, a positive result is more likely to be true. Conversely, in a community with low virus prevalence, there is a higher probability of a false positive.
Receiving a positive COVID-19 test result can be anxiety-inducing due to the potential health implications and the need to isolate from others. However, many people recover from this disease, and there are now effective treatments and vaccines available. It’s important to follow the advice of healthcare professionals, including participating in any necessary contact tracing efforts, to protect oneself and the community.
The COVID-19 testing process: how does it work?
The COVID-19 testing process is a critical component in the global response to the ongoing pandemic. It begins with a swab test, which is commonly a nasopharyngeal swab. This sample collection process involves inserting a long, flexible stick with a soft swab on the end into the back of the nasal passage through one nostril and rotating the swab several times to collect a sample from the nasopharyngeal region. This process may cause slight discomfort but is generally painless. The collected samples are then placed in a container and sent to a laboratory for analysis.
The laboratory analysis for COVID-19 primarily uses a method called reverse transcriptase polymerase chain reaction (RT-PCR). This technique identifies the virus by detecting its genetic material (RNA) in the samples. The RNA is then converted into complementary DNA (cDNA) using a process called reverse transcription. The cDNA is amplified and detected using fluorescent markers. If the virus is present in the sample, the test will be positive.
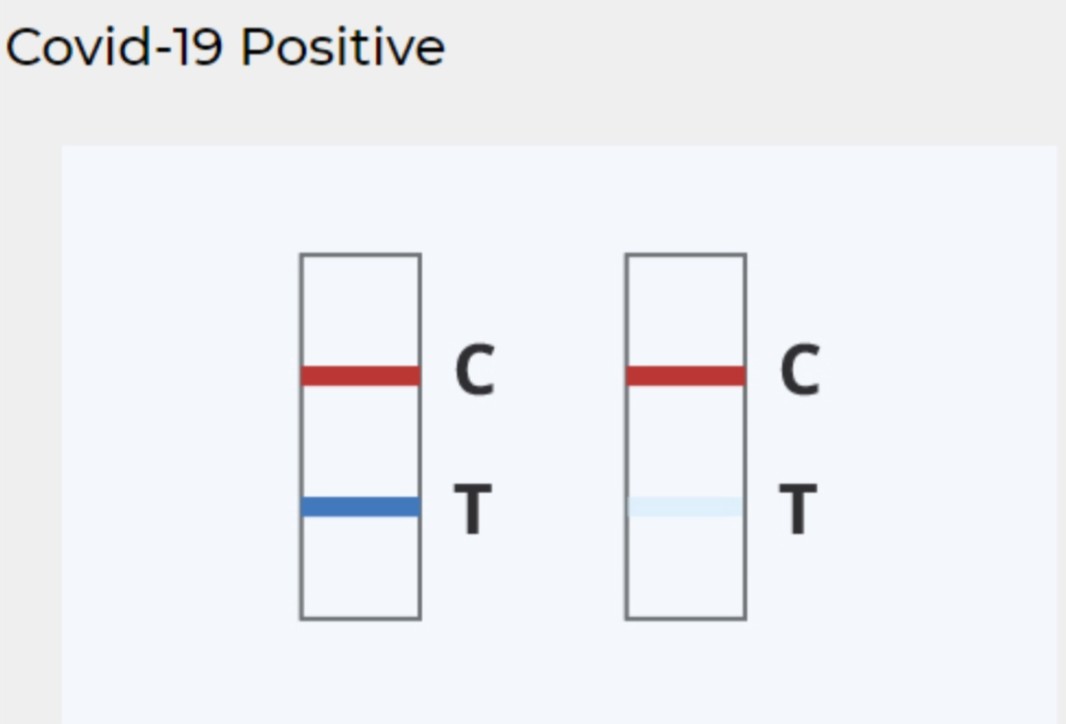
There are also rapid tests, or antigen tests, which work by identifying proteins related to the virus. These tests are faster but less reliable than PCR tests. Some rapid tests can deliver results in less than an hour, but they are more likely to miss active infection and may result in a higher percentage of false negatives. In contrast, PCR tests are more precise but can take longer, often up to a few days, depending on the laboratory’s capacity.
In addition, there are antibody tests that can identify if an individual had a past infection. These tests do not detect the virus itself, but instead, they detect antibodies the body makes in response to the virus. However, it takes a while for the body to develop these antibodies, so this test isn’t helpful for identifying current infection.
All of these tests play an integral role in understanding the spread of the virus, identifying infected individuals, and implementing appropriate measures to control the pandemic.
Frequently asked questions about false positives.
False positives are a common topic of discussion in various fields such as medicine, science, and technology. It refers to a test result indicating the presence of a particular condition, attribute, or substance when it is not actually present. In medical testing, a false positive could mean that a person is diagnosed with a disease they do not have. This can lead to unnecessary stress, additional testing and potentially harmful treatment. In technology, particularly in the field of cybersecurity, a false positive might mean that a harmless activity is flagged as potentially harmful, causing unnecessary alarm and potentially impeding productivity. It’s important to understand that while the accuracy of tests is improving over time, no test is 100% accurate and false positives can still occur. Some frequently asked questions about false positives include: How do they occur? What are the consequences? How can they be minimized? To answer briefly, false positives can occur due to errors in testing, they can lead to unnecessary stress and action, and they can be minimized through careful calibration of tests and verification of results. Understanding the concept of false positives, their occurrence, and how they can be managed is crucial in many professions today.
What should I do after a positive COVID-19 test?
Upon receiving a positive COVID-19 test, your immediate actions should primarily focus on safeguarding your health and preventing the transmission of the virus to others. Initiate a period of self-isolation and refrain from close contact with others, including those within your household, if possible. Report your test results to your healthcare provider, who can provide specific advice based on your symptoms and health history. This may include rest, hydration, over-the-counter remedies, or, in some cases, hospital care. Stay in touch with your healthcare provider and seek immediate medical attention if your symptoms wors good or become severe.
Simultaneously, inform individuals you’ve recently been in contact with about your diagnosis, allowing them to take necessary precautions and tests if needed. While you may be asymptomatic or experiencing mild symptoms, it’s crucial to remember that others, particularly those with underlying health conditions, may be more severely affected by the virus. You should also notify your workplace or school about your diagnosis to help prevent further spread.
It’s essential to take care of your mental health during this period. Remaining in isolation can be challenging, and the diagnosis may naturally lead to feelings of anxiety or stress. Connect with friends and family virtually, practice relaxation techniques, or engage in activities you enjoy to help manage these feelings.
Lastly, continue adhering to recommended guidelines including wearing a mask, washing hands frequently, and maintaining social distance even within your household. These measures can reduce the risk of transmitting the virus to others in your household. Patiently wait for your recovery, and only stop isolating when you meet the criteria set by health experts – typically, this includes waiting until at least ten days have passed since symptoms first appeared, you have had 24 hours without fever (without the use of fever-reducing medications), and other symptoms have improved. Remember, the aim is to protect yourself and those around you while you recover.
Differences between PCR tests and rapid testing tests.
PCR tests and rapid tests are two common methods employed for the detection of diseases such as COVID-19. However, they differ in several key aspects. The main variation lies in the time frame of results and the method of detection. PCR (Polymerase Chain Reaction) tests, also known as molecular tests, are typically processed in a lab and can take up to several days for the results to become available. They identify the virus’s genetic material and are generally considered to be highly accurate. On the other hand, rapid tests, also known as antigen tests, detect specific proteins on the virus’s surface. These tests are often done on-site and can provide results in as little as 15 minutes. However, they are usually less accurate than PCR tests and may require a PCR test for confirmation in the case of a negative result. The choice between the two tests often depends on the situation. For instance, rapid tests might be used for mass screening in a community or large group setting, while PCR tests are typically used for individuals showing symptoms or have had close contact with a confirmed case. Both tests play crucial roles in disease control and prevention, helping to identify infected individuals and curb the spread of the virus. As such, the most effective testing strategy often involves a combination of both PCR and rapid tests, tailored to the specific needs and conditions of the situation.
How can I protect others after a positive COVID-19 test?
In the event of receiving a positive COVID-19 test result, there are several prudent measures to adopt to safeguard others from potential infection. Primarily, it is essential to immediately isolate oneself. This means staying at home and avoiding contact with other individuals as much as possible, including those living in the same household. If it is necessary to interact with others, ensure it is done wearing a mask and maintaining a safe distance.
Secondly, ensure to inform individuals you have had contact with about your positive result. This is crucial in allowing them to monitor their health for symptoms and seek testing if necessary, thereby preventing potential further spread of the virus. This includes both personal and professional contacts.
Additionally, maintaining hygiene becomes significantly important. Regular hand washing and sanitizing surfaces you have touched can help prevent the virus from spreading. If you share a living space with others, use a separate bathroom if available and avoid sharing personal items such as towels, dishes, and bedding.
Consider seeking medical advice as well. Health professionals can provide guidance tailored to your specific circumstances, such as the severity of your symptoms and any underlying health conditions. They can advise when you are no longer infectious and can safely end your isolation.
Furthermore, if you have traveled recently, report your positive result to the relevant authorities. This can aid in contact tracing efforts, helping to identify and inform others who may have been exposed during your travels.
Lastly, maintain your health through proper nutrition, hydration, and rest. This will not only aid your recovery but also mitigate the risk of severe symptoms that could necessitate medical intervention and potential exposure of healthcare workers.
Adopting these measures can effectively help protect others after a positive COVID-19 test. This is a collective responsibility we all hold in the fight against the ongoing pandemic.